For in-person services, there are several locations around and
beyond the Tacoma area.
For deliveries, please call by 10am for assistance.

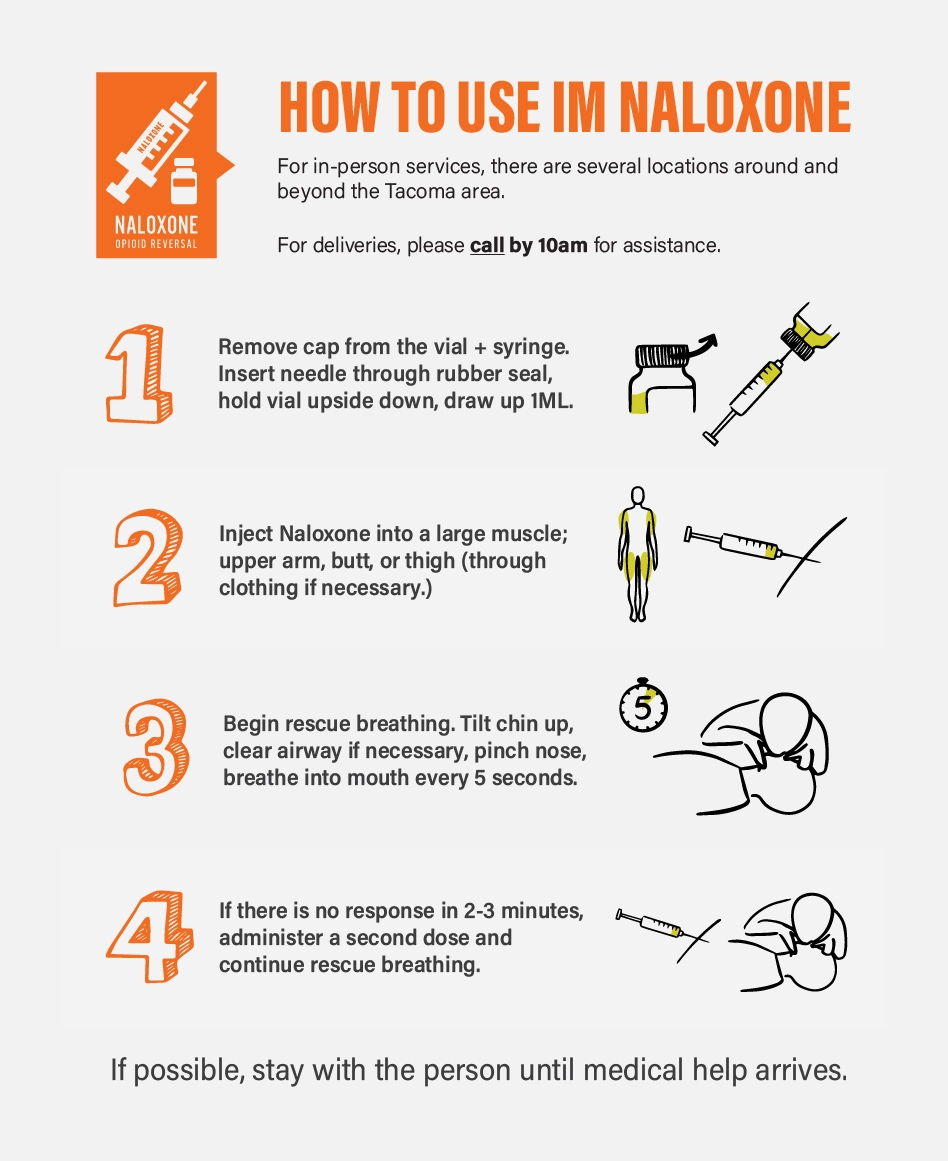

CLICK HERE FOR IM NALOXONE INSTRUCTIONS
+

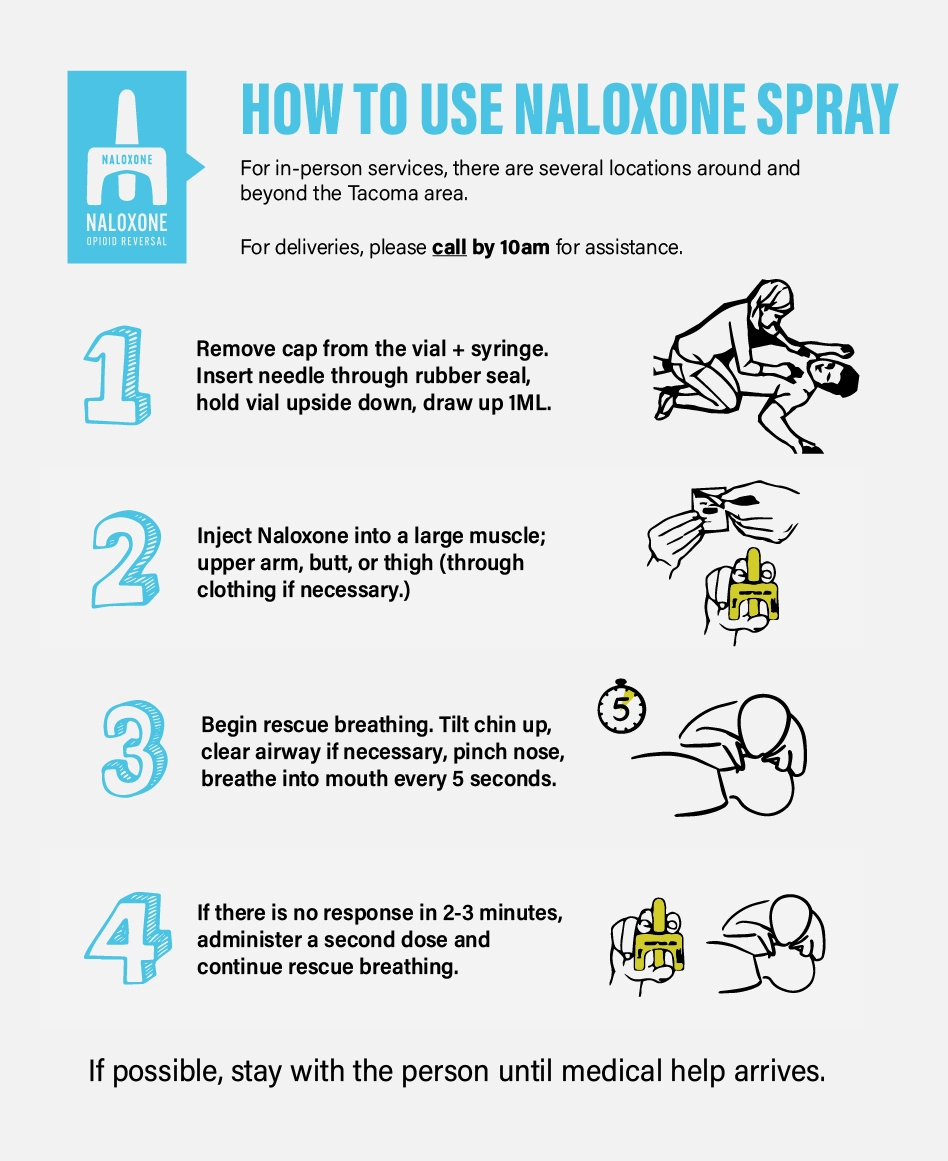
CLICK HERE FOR NALOXONE SPRAY INSTRUCTIONS
+
This video provides a step-by-step guide on how to use Naloxone (Narcan) to reverse an opioid overdose. It covers when and how to administer the medication, signs of an overdose, and what to do after giving Naloxone. Learn how to act quickly and confidently in an emergency situation to save a life.

How do I rouse an unconscious person?
If you find someone unconscious and suspect an overdose:
2. Check for breathing and responsiveness:
3. Administer naloxone (Narcan):
4. Provide rescue breathing if needed:
5. Stay until help arrives:
Naloxone wears off in 30–90 minutes, and the person can go back into overdose as naloxone does not remove drugs from a person's body.
Try to keep them awake and monitor their breathing.
Should I put them in a cold shower?
No, you should NEVER put someone who is overdosing into a cold shower. Here’s why:
Why cold showers are dangerous during an overdose:
What to do instead:
Should I make them vomit?
No, you should not try to make someone who is overdosing vomit. Here’s why:
How many different forms of naloxone are available?
There are three main forms of naloxone commonly used in the U.S., each with its own method of delivery. The Tacoma Needle Exchange provides the first two listed below at all of our exchange sites and the nasal naloxone via vending machines throughout Pierce County, Washington.
1. Nasal Spray (Narcan, generic naloxone spray)
2. Injectable Naloxone (vials or ampoules)
3. Auto-Injector (EVZIO — discontinued in the U.S. but still sometimes seen)
